Managing a Bruised Toenail

A bruised toenail, or subungual hematoma, occurs when trauma to the toe causes blood to pool underneath the nail. This can result from dropping a heavy object on your foot, repetitive impact from activities like running, or wearing shoes that apply excessive pressure to the toenails. Symptoms of a bruised toenail include pain, discoloration ranging from dark red to black, a feeling of pressure under the nail, and, in some cases, nail detachment. While minor toenail bruising may resolve itself over time, larger hematomas can increase the risk of infection or permanent nail deformities. A podiatrist can assess the severity of the injury and provide treatment options. Included are draining the trapped blood to relieve pressure or, in more severe cases, performing surgery to prevent complications. If an infection develops or the nail becomes chronically damaged, additional care may be required to promote proper healing and nail regrowth. If you have a bruised or discolored toenail, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and appropriate treatment options.
Toe pain can disrupt your daily activities. If you have any concerns, contact Dr. Mark Gagnon of Advanced Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toe Pain
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.
Pressure Sores Can Lead to Foot Ulcers
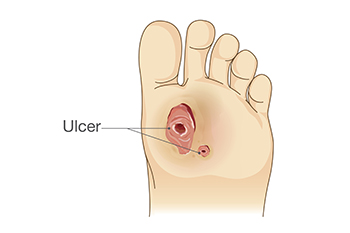
Rubbing points, also termed pressure sores, on the feet, toes, or ankles can progress into serious foot ulcers if left untreated. These pressure sores develop when prolonged pressure reduces blood flow, damaging the skin and underlying tissues. People with health conditions that impair circulation, such as diabetes or vascular disease, face a higher risk. Pressure sores are classified by severity, starting as red, painful skin and potentially worsening into deep wounds that expose muscle or bone. Common rubbing sites include the heels and bony areas of the foot. Without proper care, these wounds may become infected, further complicating healing. A podiatrist can assess the severity of a pressure sore and recommend appropriate treatment to prevent complications. This may involve wound care, pressure relief strategies, specialized dressings, or in severe cases, surgery to remove damaged tissue. Regular monitoring and professional treatment are essential to reduce the risk of infection and promote healing. If you have foot sores that are not healing properly, it is suggested that you schedule an appointment with a podiatrist for wound care treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Mark Gagnon from Advanced Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Symptoms and Causes of Chronic Ankle Pain

Chronic ankle pain is a condition that persists over time and can significantly impact a person’s mobility and quality of life. This type of pain often results from previous injuries, such as sprains or fractures, that have not healed properly or have led to long-term damage. Symptoms include persistent pain, swelling, stiffness, and a limited range of motion, especially after physical activity. Individuals may also experience instability or the feeling that their ankle might give way. The causes of chronic ankle pain can vary, but they are commonly linked to repeated ankle sprains, improper rehabilitation, or overuse. Conditions like tendonitis, arthritis, or even cartilage damage can also contribute to the ongoing discomfort. In some cases, biomechanical issues, such as abnormal foot alignment or muscle imbalances, may worsen the problem. Relief typically involves a combination of rest, and, in some cases treatment may include surgery to address the underlying issue. If you have chronic ankle pain, it is suggested that you make an appointment with a podiatrist for a diagnosis and treatment.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with Dr. Mark Gagnon from Advanced Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Pain
The ankle joint is the point at which the bones of the leg and foot join. This joint is crucial because it is responsible for the foot’s mobility. Ankle pain is typically the result of inflammation from an injury to bones, joint space, cartilage, ligaments, tendons, or muscles in the area. Commonly associated symptoms with ankle pain are bruising, redness, numbness, stiffness, weakness, and tingling.
The most common causes of ankle pain are sprains and injuries. Ankle sprains are one of the most common musculoskeletal injuries. Sprains occur when the ligaments of the ankle become partially or completely torn due to sudden stretching. Sprains can occur on either the inner or outer sides of the ankle joint. Usually, these injuries occur when the ankle is twisted in an activity by stepping off an uneven surface. More specific causes include rheumatoid arthritis, gout, osteoarthritis, and Achilles tendonitis.
If you are experiencing ankle pain, you should consult with your podiatrist to choose the best method of care. Your doctor will conduct an examination of your ankle to determine the underlying cause of the pain.
Wounds That Don't Heal Need to Be Checked
Ankle-Foot Orthoses for Stroke Patients

Ankle-foot orthoses, or AFOs, can help stroke survivors improve their walking ability. They are devices worn on the lower leg and foot to support movement. Passive AFOs provide stability and hold the foot in a fixed position to prevent dragging and tripping. Dynamic AFOs, on the other hand, offer more flexibility, allowing smoother motion during walking. These devices are especially helpful for individuals with plantar flexor, or lower leg muscle weakness, which are involved in the push-off phase of walking. By improving alignment and control, AFOs make walking easier and safer, reducing the risk of falls. Each type of AFO is designed to address different needs, so the right choice depends on the individual. If you have had a stroke and want to improve your walking ability, it is suggested that you schedule an appointment with a podiatrist who can assess your condition, recommend the most suitable orthotic, and ensure it fits comfortably for the best results.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. Mark Gagnon from Advanced Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
Common Foot Changes During Pregnancy

During pregnancy, a woman’s body undergoes significant changes that often affect the feet, toes, and ankles. Hormonal shifts relax ligaments, which can lead to developing flat feet and causing overpronation, which can result in discomfort or balance issues. Increased weight and a growing uterus place extra stress on the arches, potentially resulting in heel pain. Swelling in the feet and ankles is caused by increased blood volume and fluid retention, which may make shoes feel tighter. Changes in nail health, such as brittleness or ridges, are also frequently observed. Foot changes during pregnancy can be worsened by prolonged standing or improper footwear. A podiatrist can assess and address these concerns by recommending appropriate footwear, custom orthotics, and professional care for swelling or nail-related conditions. While many changes resolve after the baby is born, some may persist, and timely attention can prevent further complications. If you are experiencing foot discomfort during pregnancy, it is suggested that you make an appointment with a podiatrist for a diagnosis and necessary treatment.
Pregnant women with swollen feet can be treated with a variety of different methods that are readily available. For more information about other cures for swollen feet during pregnancy, consult with Dr. Mark Gagnon from Advanced Podiatry. Our doctor will attend to all of your foot and ankle needs.
What Foot Problems Can Arise During Pregnancy?
One problem that can occur is overpronation, which occurs when the arch of the foot flattens and tends to roll inward. This can cause pain and discomfort in your heels while you’re walking or even just standing up, trying to support your baby.
Another problem is edema, or swelling in the extremities. This often affects the feet during pregnancy but tends to occur in the later stages.
How Can I Keep My Feet Healthy During Pregnancy?
- Wearing orthotics can provide extra support for the feet and help distribute weight evenly
- Minimize the amount of time spent walking barefoot
- Wear shoes with good arch support
- Wear shoes that allow for good circulation to the feet
- Elevate feet if you experience swelling
- Massage your feet
- Get regular, light exercise, such as walking, to promote blood circulation to the feet
If you have any questions please feel free to contact one of our offices located in Crestwood, Orland Park, and Summit, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.